Understanding Hamstring Strain Injuries

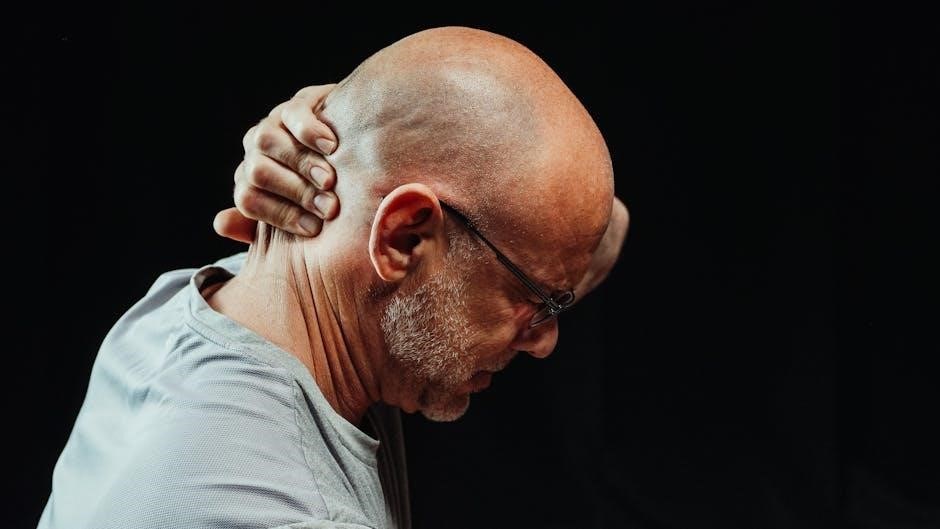
Hamstring strain injuries are a common issue in sports, requiring a comprehensive rehabilitation approach. Understanding the injury’s nature, grading, and appropriate rehabilitation protocols is essential for optimal recovery and return to activity. Early diagnosis and tailored treatment plans, including physical therapy and progressive exercises, ensure effective healing and prevent future injuries.
Overview of Hamstring Strain Grades
Hamstring strains are classified into three grades based on severity. Grade 1 involves mild micro-tears of the muscle fibers, causing pain but no significant loss of strength or function. Grade 2 is a partial tear with more pronounced pain, swelling, and limited mobility. Grade 3 is a complete rupture of the muscle-tendon unit, leading to severe pain, swelling, and inability to contract the muscle effectively. Accurate grading is crucial for developing targeted rehabilitation protocols. Early identification of the grade ensures appropriate treatment, reducing the risk of prolonged recovery or recurrence. Understanding the grade also helps in setting realistic expectations for recovery timelines and return-to-sport readiness. Each grade requires a tailored approach, emphasizing pain management, progressive strengthening, and functional exercises to restore optimal hamstring function and prevent future injuries.
Clinical Presentation and Diagnosis
Hamstring strains typically present with sudden, sharp pain at the back of the thigh during activity, often accompanied by swelling, bruising, or muscle spasms. Patients may report a “pop” or tearing sensation at the time of injury. Physical examination reveals tenderness along the affected muscle, with pain worsening during resisted knee flexion or hip extension. The bent-knee stretch test is commonly used to assess hamstring integrity. Diagnosis is primarily clinical, supported by patient history and physical findings. Imaging, such as MRI, is reserved for severe cases to confirm the extent of muscle or tendon damage. Early and accurate diagnosis is critical for guiding appropriate treatment and preventing complications. Proper assessment ensures the development of a tailored rehabilitation protocol aligned with the injury’s severity and the patient’s functional goals.

Clinical Assessment and Evaluation
Clinical assessment involves a thorough physical exam, including palpation, range of motion, and strength testing. Specific tests like the bent-knee stretch test help confirm hamstring injury severity and guide rehabilitation planning effectively.
Physical Examination Techniques
Physical examination techniques for hamstring strain injuries involve palpation to identify areas of tenderness and swelling. Range of motion assessments, including knee flexion and hip extension, are performed to evaluate flexibility and pain. Strength testing, such as resisted knee flexion, helps determine the extent of muscle weakness. Special tests like the bent-knee stretch test and slump test are used to assess neural tension and hamstring tightness. These findings guide the development of a personalized rehabilitation protocol and help monitor progress throughout the recovery process. Accurate physical examination ensures appropriate intervention and minimizes the risk of further injury or prolonged recovery times.
Diagnostic Tests and Imaging
Diagnostic tests and imaging are crucial for confirming the extent of hamstring strain injuries. Magnetic Resonance Imaging (MRI) is the gold standard for evaluating muscle and tendon damage, providing detailed images of soft tissue injuries. It helps identify partial or complete tears, muscle edema, and tendon involvement. Ultrasound is also used for dynamic assessments, offering real-time visualization of muscle function and guiding injections or other interventions. Clinical tests, such as the bent-knee stretch test and slump test, are often combined with imaging to confirm diagnoses. These tools ensure accurate severity assessment, guiding tailored rehabilitation protocols and monitoring recovery progress effectively.

Prevention Strategies for Hamstring Strains
Preventing hamstring strains involves comprehensive warm-ups, dynamic stretching, and targeted strengthening exercises. Implementing injury-specific protocols and ensuring proper recovery reduces the risk of recurrence and enhances overall muscle resilience.
Warm-Up and Stretching Routines
A proper warm-up and stretching routine are critical for preventing hamstring strains. Begin with a dynamic warm-up, such as cycling or brisk walking, for 10-15 minutes to increase blood flow and muscle temperature. Incorporate dynamic stretches like leg swings, high knees, and lunges to improve flexibility and range of motion. Focus on static stretches, such as the supine 90/90 hamstring stretch and lunging hip flexor stretch, to target the hammies and surrounding muscles. Perform these stretches post-exercise when muscles are warm to maximize effectiveness. Include isometric exercises, like hamstring isometrics, to strengthen the muscles without movement. Aim for 3 sets of 15 repetitions, 3 times daily, to enhance muscle elasticity and reduce injury risk. Consistency in these routines is key to maintaining muscle health and preventing strains.
Strengthening Exercises for Injury Prevention
Strengthening exercises are vital for preventing hamstring strains. Begin with foundational exercises like hip bridges and knee flexions to target the hamstrings and glutes. Progress to resistance-based exercises, such as hamstring curls using a Swiss ball or resistance bands, to build muscle endurance. Incorporate functional exercises like step-ups and deadlifts to improve strength in real-world movements. Ensure exercises are performed with proper form to avoid strain. Start with low loads and gradually increase intensity as strength improves. Focus on eccentric exercises, which target the lengthening phase of muscle contractions, a key factor in hamstring function. Perform 3-4 sets of 8-12 repetitions for each exercise, 3-4 times weekly. Consistency in these routines enhances muscle resilience, reducing the risk of future injuries and improving overall athletic performance.
Acute Management of Hamstring Strains
Acute hamstring strain management focuses on reducing pain and inflammation. Apply the RICE principle: Rest, Ice, Compression, and Elevation. Pain management and early mobilization are critical for proper recovery.
Pain Management and Inflammation Control
Effective pain management and inflammation control are critical in the acute phase of hamstring strain rehabilitation. The RICE principle—Rest, Ice, Compression, and Elevation—is essential to minimize swelling and pain. Ice should be applied for 15–20 minutes every 2–3 hours during the initial 48–72 hours post-injury. Compression sleeves or elastic bandages can help reduce edema. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to alleviate pain and inflammation. Gentle, pain-free exercises, such as isometric contractions and passive stretching, can be introduced early to maintain muscle function without exacerbating the injury. Modalities like ice or GameReady therapy are often recommended to manage post-exercise soreness. Early intervention ensures proper healing and prevents complications, setting the foundation for progressive rehabilitation.
Early Mobility and Range of Motion Exercises
Early mobility and range of motion exercises are vital to prevent stiffness and promote recovery after a hamstring strain. Gentle exercises, such as supine 90/90 hamstring stretches and lunging hip flexor stretches, help maintain flexibility without overloading the injured tissue. Isometric hamstring contractions and passive stretching are introduced early to preserve muscle function. These exercises should be performed within a pain-free range to avoid aggravating the injury. Progression to active knee extensions and heel slides is recommended as symptoms improve. Early mobilization enhances blood flow, reduces muscle atrophy, and prepares the hamstring for more dynamic movements later in rehabilitation. Supervised exercises ensure proper technique and gradual progression, minimizing the risk of re-injury while restoring normal mobility.

Rehabilitation Protocol for Hamstring Strains
A structured, multi-phase approach focusing on strength, flexibility, and functional progression is key to hamstring strain rehabilitation, ensuring a safe return to sport and activity.
Progressive Strengthening Exercises
Progressive strengthening exercises are a cornerstone of hamstring strain rehabilitation. These exercises aim to restore muscle strength, endurance, and power while minimizing the risk of re-injury. Early stages focus on isometric exercises, such as hamstring contractions and bridging, to activate the muscles without putting excessive strain on the tissues. As the injury heals, resistance is gradually introduced using bands, weights, or machines. Eccentric exercises , which emphasize the lengthening phase of muscle contraction, are particularly effective for hamstrings. Examples include deadlifts, leg curls, and step-ups. The exercises are progressed based on pain-free movement and strength improvements. Proper form and technique are emphasized to ensure safe and effective loading of the hamstrings. A physical therapist can tailor the program to address individual needs and facilitate a smooth transition to functional activities. Consistency and adherence to the protocol are critical for optimal recovery and return to sport.
Flexibility and Stretching Program
A well-structured flexibility and stretching program is essential for restoring hamstring function after an injury. Gentle, static stretches are introduced early to improve range of motion and reduce muscle stiffness. Examples include the supine 90/90 hamstring stretch and lunge hip flexor stretch. These exercises are typically held for 20-30 seconds and repeated 2-3 times. As the injury progresses, dynamic stretches like leg swings and high knees are incorporated to mimic functional movements. Hamstring-specific isometrics, such as seated hamstring holds, can also enhance flexibility without overloading the muscle. Stretching exercises are performed 2-3 times daily, focusing on pain-free movements. A physical therapist can tailor the program to address individual limitations and ensure proper technique. Consistency in the stretching routine is crucial for achieving long-term flexibility and reducing the risk of recurrence; This program complements strengthening exercises to promote a full recovery.
Agility and Functional Drills
Agility and functional drills are integral to the later stages of hamstring strain rehabilitation, focusing on restoring dynamic movement patterns and sport-specific skills. These drills aim to improve reaction time, speed, and coordination while minimizing the risk of re-injury. Examples include figure-eight runs, shuttle runs, and zigzag drills, which mimic real-world movements. Progression involves increasing intensity, such as adding sudden changes of direction or incorporating resistance bands. Functional drills like single-leg hops and balance exercises enhance stability and proprioception. These exercises are tailored to the individual’s sport and specific demands, ensuring a smooth transition back to competitive activity. Supervised by a physical therapist, agility drills are introduced once strength and flexibility milestones are achieved, ensuring the hamstring muscles are prepared for high-level functional demands and reducing the likelihood of future injuries.

Criteria for Progression and Return to Sport
Progression and return to sport are guided by objective criteria, including clinical markers, strength, flexibility, and functional assessments. Athletes must demonstrate readiness through pain-free performance and functional tests.
Objective Criteria for Rehabilitation Progression
Objective criteria for rehabilitation progression include measurable improvements in strength, flexibility, and functional capacity. Athletes must achieve specific milestones, such as pain-free range of motion, normalized strength compared to the uninjured side, and functional movement patterns. Clinical assessments, like single-leg deadlifts or bridge tests, evaluate readiness for advanced exercises. Progression is also based on the absence of pain or discomfort during activities and the ability to perform sport-specific movements with proper mechanics. Additionally, strength and power metrics, such as hamstring-to-quadriceps ratios, are used to ensure safe progression. These criteria minimize the risk of re-injury and ensure a structured, evidence-based approach to rehabilitation. Clinical judgment and individualized care remain central to achieving optimal outcomes.
Return-to-Play Readiness Assessment
A comprehensive return-to-play readiness assessment ensures athletes are prepared for sport-specific demands post-injury. This evaluation includes functional movement screens, strength testing, and sport-specific drills to confirm readiness. Athletes must demonstrate pain-free performance in activities like sprinting, cutting, and changing direction. Strength metrics, such as hamstring-to-quadriceps strength ratios, are assessed to ensure muscle balance and reduce re-injury risk. Additionally, agility drills and high-speed movements are used to mimic game conditions. Psychological readiness and confidence in performing sport-specific tasks are also evaluated. The assessment ensures a safe and gradual transition back to competition, minimizing the likelihood of re-injury and optimizing performance. These criteria are critical for determining when an athlete can safely resume play at pre-injury levels.
